As patients in the central San Joaquin Valley scramble to receive health care services following the abrupt shuttering of Madera Community Hospital, a sizable swath of patients will be unable to access Community Regional Medical Center, Clovis Community Medical Center, or doctors within the Community Health Partners network under their insurance plans.
Community issued a formal termination of its Contracting Hospital Agreement with Anthem, UnitedHealthcare, and Cigna, a move that extends to restricting patient access to members of its doctor group.
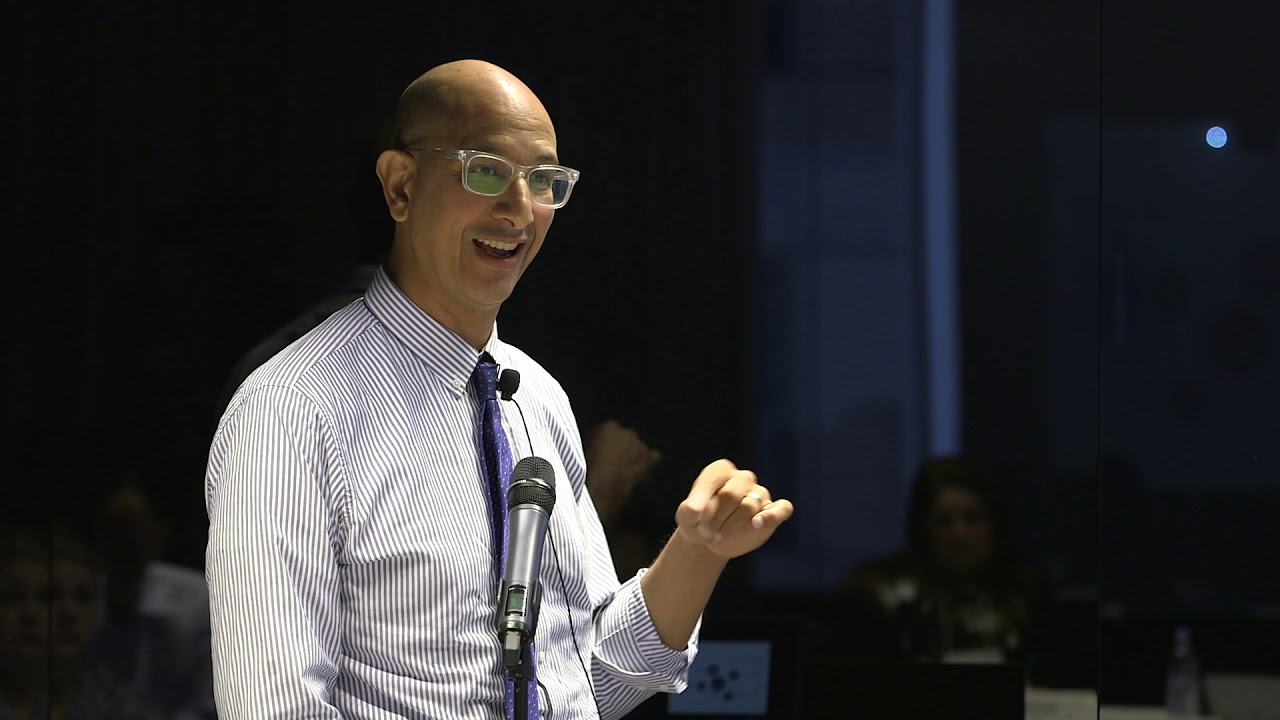
What they’re saying: Aldo De La Torre, Community’s Senior Vice President of Network Development and Insurance Services, shuffled blame to insurers for failing to adjust reimbursement rates to account for COVID-19 impacts and inflationary trends. Asked about Anthem, the largest of the trio by customer base, he issued the following statement:
- “Community Health System is committed to continuing to deliver the comprehensive, accessible care that our region deserves. However, we must require fair, sustainable reimbursement rates from health plans so that we remain financially viable in the long term.
While we have made progress in our negotiations with other health plans, we have reached an unfortunate impasse in our negotiations with Anthem. The last time Community entered into negotiations with Anthem was in 2019, prior to the existence of the COVID-19 pandemic. Anthem has offered rate increases that are far less than even general inflation trends, and does not account for increased costs of delivering care in our current, extremely challenging environment.
Anthem is a for-profit insurance company that has continued to raise rates—offering very little additional compensation to providers of care. Keeping premiums for profits, not for care, should be unacceptable to their members. Again, we are asking Anthem to work with us to renew a fair and sustainable agreement.”
Anthem representatives did not respond to calls from The Sun.
If history is any guide… Sources told The Sun that Anthem patients could be in for a long wait for a resolution between the hospital and insurer.
Its last contract negotiation, inked in 2019 took months to resolve, forcing patients to file for continuance of care with their physicians under Community Health Partners, the hospital’s proprietary doctor group.