Yes, there’s been a pandemic
In early January 2020, reports of a deadly new disease that originated in China began circulating around the world. In a matter of weeks, it had spread to nearly every continent and infected 3.8 million people, leaving more than 265,000 people dead. This strange new virus, COVID-19, spread quickly and preyed on the vulnerable, as evidenced by its path of destruction throughout the world. The initial estimate by experts was a death rate of around 3% – close to 10 million Americans dead. Experts at the CDC suggested that the number of sick patients would rapidly overwhelm our hospitals. That was the original logic behind quarantine and social distancing. Despite this, new numbers suggest that COVID-19 is far less deadly than experts previously believed.
Flatten the Curve, the Rationale Behind the “Lockdown”
On March 11, President Trump closed the borders to travel from Europe. Eight days later, California’s governor Gavin Newsom announced that the state would implement an indefinite shelter-in-place. Three days after that, Governor Andrew Cuomo shut down New York. At the time, these leaders were taking the steps they thought appropriate due to a lack of information about COVID-19. The initial reports from Italy and Spain were horror stories and soon thereafter we saw an uptick in patients in New York City. Faced with such a situation, we believed a lockdown was necessary for information-gathering. Dr. Fauci said that the initial numbers estimated 10 million Americans dead. These shutdowns were implemented in an attempt to flatten the curve so that our hospitals weren’t overwhelmed. Yet even at its highest peak, New York City’s hospitals were not overwhelmed.
We were initially told that the U.S. infection rate was increasing exponentially. But those data were based on a simple fallacy: the number of new cases went up at, approximately, the same rate that new tests were performed. It was a linear increase until the testing number reached 100,000 daily tests. Since then, there has not been a significant increase in the number of testing, nor a significant increase in the number of new cases. New case numbers fluctuate between 30,000, plus or minus 5,000 cases depending on the number of tests being conducted.
People praise California for its lockdown and social distancing practices, although it implemented the policies only three days before New York City. The problem with the data coming out of California is the number of people being tested. California has 1/10 of the deaths of New York but California has only done 1/10 of the testing that New York has. California is attributing it all of its success to the lockdown, but that isn’t the entire story. The ratio of infections to tests in New York and California are nearly identical. This emphasizes the recent Stanford and USC studies that show that the virus is more prevalent in California than perceived.
That being said, we did not have a complete lockdown, not even in New York. New York City’s subway is still running. Instead, we had a pseudo-lockdown that only affected some people in some states. People whose jobs were deemed “essential” kept their jobs. These individuals would go to work, pick up COVID-19, and then bring it home to their non-essential partners. Certain businesses were also deemed essential, and, because they had nothing else to do, “non-essential” people bored at home would cram into these essential businesses every day. In doing so, these non-essential shoppers increased the likelihood of picking up the pathogen and bringing it home to their families. The United States did not have a lockdown and we’re fooling ourselves if we think we did.
Lockdowns Likely Didn’t Help
Governor Cuomo, on May 6, 2020 acknowledged that 66% of all COVID-19 cases in New York City were quarantined and practiced social distancing. Those of us who have been pushing for a lockdown will pat ourselves on the back once the numbers begin coming down. However, based on data from China, South Korea, Italy, and Spain, the numbers will peak from 30-38 days after infection, regardless of the lockdown measures. This is a form of confirmation bias. It wasn’t our pseudo-lockdown that drove down numbers—it was just the natural course of the pathogen. Two weeks into the lockdown, Dr. Fauci and his colleagues announced that the initial data was incomplete and new data suggested that the mortality rate was inflated by 5,000 percent. From initially 10 million Americans dead, we are now looking at 60,000 – 100,000; this figure uses the liberal coding of deaths as attributable to COVID-19, as Dr. Deborah Birx admitted. During the same press conference, they mentioned that the number of hospital visits was grossly overestimated and that the reasoning behind the lockdown, which was hospital bed availability, was no longer valid. No course correction about policies were made at that point.
The Mortality Rate Continues to Fall
A recent Stanford study suggests that we are undercounting the number of people infected by this disease by a factor of 50-80. People accused the researcher of being biased because he was one of the original scientists who questioned the virus’s deadliness. Less than a week after the Stanford study was released, however, a USC study confirmed those same findings, and the following week, researchers at Massachusetts General Hospital conducted a random blood sample study that suggested 1/3 of Massachusetts residents have already seen this virus and have produced antibodies. Some people who showed that they had been exposed to the virus didn’t even report feeling sick. We can’t assume that those who have antibodies are protected, but we can safely assume that they have been exposed to the virus.
The USS Theodore Roosevelt has been a petri dish for COVID-19 among its sailors. The aircraft carrier has a crew of over 4,800 and 600 of them became ill with COVID-19. Of those 600, only one tragically died. That sailor’s death is a national tragedy, but it offers some insight into the fact that a young and healthy demographic is not at a high risk for death from COVID-19.
Women who were going into labor in New York City were being tested for COVID-19. In this group, 15% of women tested positive for COVID-19 and 80% of patients with positive test results were asymptomatic. If they hadn’t come to the hospital to have a baby, they never would have known they had COVID-19.
Iceland did a random testing of its population, and the results suggest that half of the antigen-positive individuals were asymptomatic.
These data suggest that we are underestimating the number of people impacted by COVID-19, which has several ramifications. One is that the infection fatality rate of this disease is actually 10-30 times less than we originally thought: COVID-19 is slightly, by a factor of 1.5 to 2 times, deadlier than the annual flu. Second, these tests indicate that we are not in the initial or the plateau stage of the infection. Therefore, the policies of contact tracing are impossible and unnecessary at this time. Based on CDC data from last year, the seasonal flu accounted for 490,600 hospitalizations and 34,200 deaths. This gives a case fatality rate for hospitalizations for the flu, approximately 7%.
Currently, the case fatality rate of hospitalized patients for COVID-19 is around 5%. This is an important distinction to make. As more community antibody testing is being done, we realize that a great majority of patients with this disease are either asymptomatic or mildly asymptomatic. As mentioned above, this will bring a fatality rate of this virus to roughly the same level as the flu virus.
Important Statistics About Demographics that are Mostly Affected by COVID-19
Unless a viable vaccine is on the horizon, which it doesn’t appear to be, the only purpose of lockdown is to ensure hospital bed availability. Most hospitals in the United States are operating at 40% capacity.
The area underneath the curves are the same. This means that the same number of people will get sick from the virus. The mitigation curve just spreads the number of sick over a longer period of time to ensure that there is hospital availability.
A Deadly Disease for the Elderly
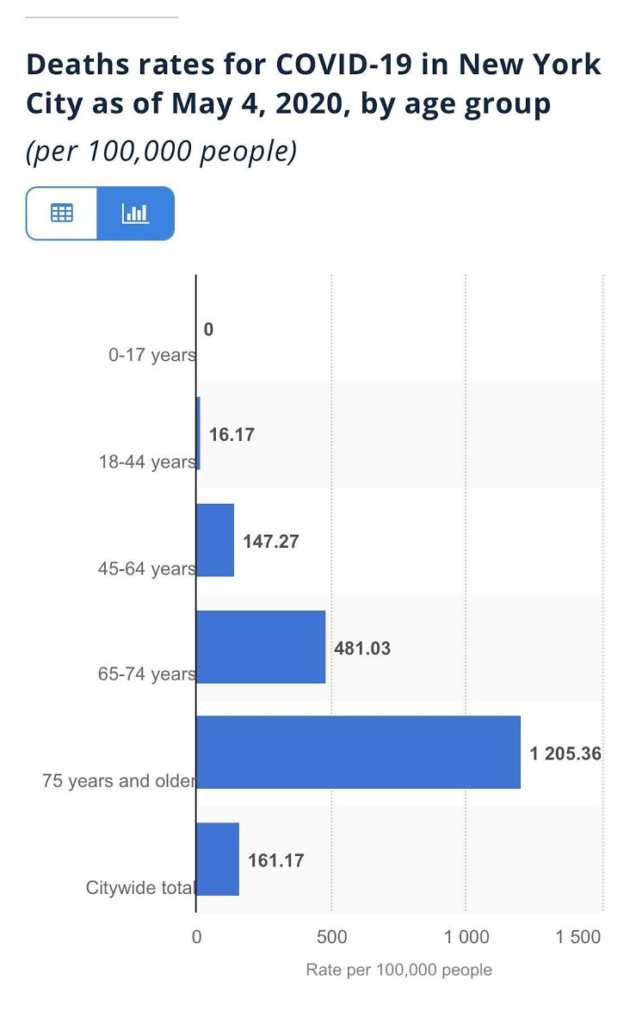
The studies out of Italy, which was hit just as hard as New York City, show that the median age of death was 79.5 years old. This disease mostly affects those over 65 and those with other underlying health conditions. Yes, it has killed those under the age of 50, but that’s not the majority.
As of May 6, 2020, less than 1,000 Americans under the age of 50 have died from COVID-19. Last year 3,500 Americans under the age of 50 died from the flu.
People over the age of 65 are the ones that are mostly affected by this. Mortality rates of those under age 50 is far below 0.1%. This disease will continue until herd immunity is reached or a vaccine is created. As data suggests, it has not slowed down in the United States based on the policies enacted thus far.
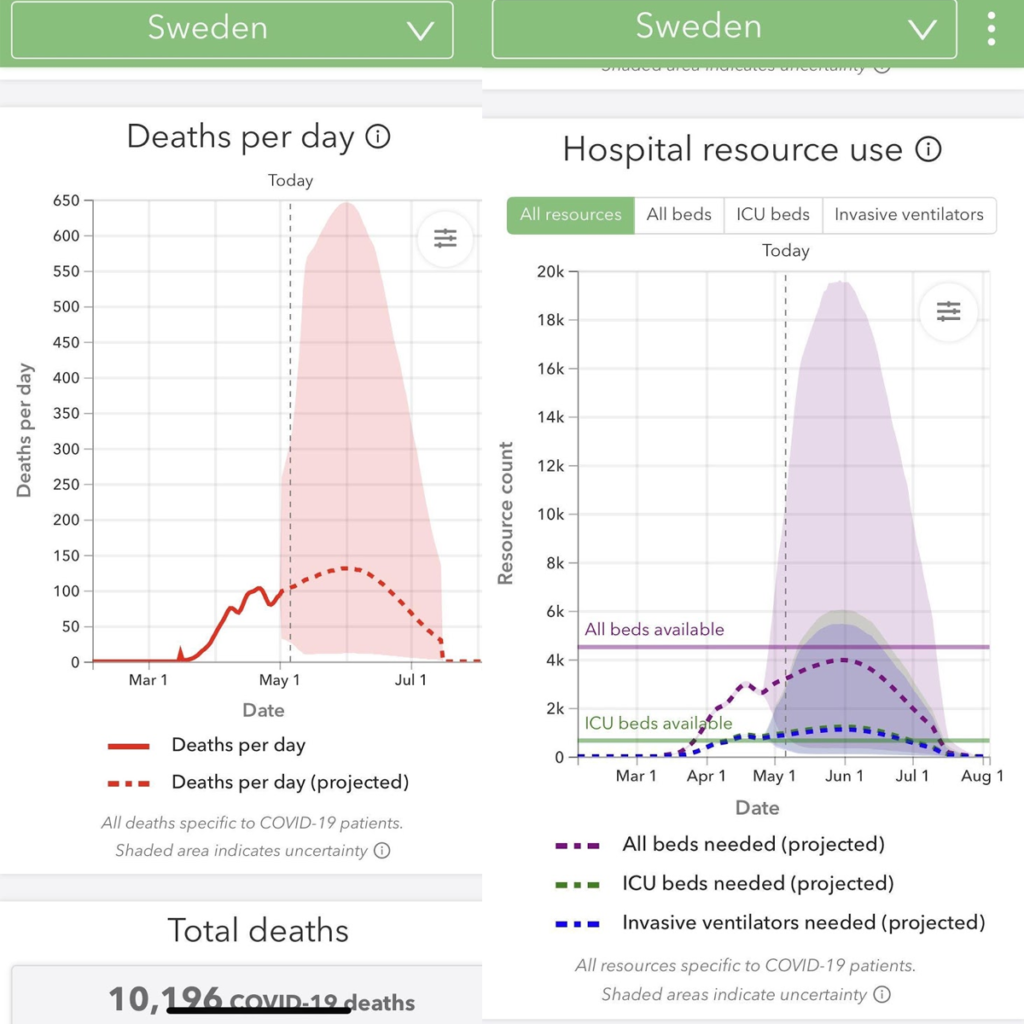
A Different Approach – The Swedish Experiment
Sweden took a different approach. They decided to keep businesses open and ask the elderly and those with medical conditions to self-quarantine. Initially, death rates per million in Sweden were high, but still not as high as New York or Detroit. Sweden’s numbers have now plateaued and are on their way down. The health minister of Sweden recently stated that the country will reach herd immunity by the end of May. Sweden’s approach doesn’t mean it doesn’t care about the elderly or those at risk – it means the exact opposite. Allowing the young and healthy to work builds herd immunity as soon as possible and actually protects the young and vulnerable while maintaining economic prosperity. In the long run this will save countless lives. As of May 6, 2020, Sweden has had 2,940 deaths, and 24,000 cases.
As the graphs below show, the models that suggested that without mitigation the number of deaths will be extremely high were wrong. Data suggests that even without a draconian lockdown, Sweden, just like New York City, will not exceed its hospital bed capacity. The Swedes decided to quarantine the elderly and sick, keep the economy open, allow the young to go to school, and let adults without medical conditions to go to work, restaurants, etc. In the process, they are on the road to recovery and achieving herd immunity. Furthermore, the graphs suggest that Sweden’s worst days are behind it but the United States continues to have the same number of daily infections and deaths.
We are not suggesting that Sweden and the United States have the same demographic, population densities, access to care, etc. The United States is not Sweden but by the same token, the rest of the United States, especially rural America, is not New York City. Uniform policies that may or may not work in New York City should not apply to the rest of the country. Each state, county, and locality should be evaluated based upon its own needs.
Other countries like Singapore, Taiwan, and Hong Kong were initially hailed as heroes for doing all the right things. These countries locked down swiftly and implemented social distancing. As it stands now, Singapore, Hong Kong, and Taiwan are facing their second wave of cases. During an interview with Singapore’s health minister, he acknowledged that they are currently facing a second wave of this attack and he said that these waves will continue until herd immunity is reached.
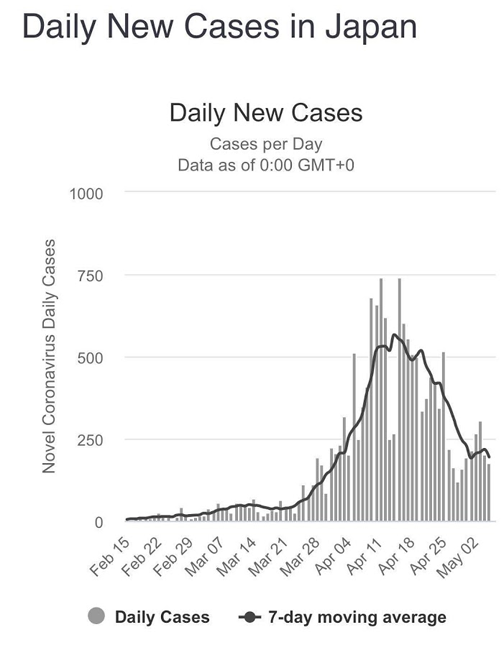
Japan’s approach was similar to Sweden’s. The doctor leading Japan’s decisions, Shigeru Omi, advises Prime Minister Shinzō Abe for the coronavirus. He made the decision to not implement a countrywide lockdown, saying that elimination of the virus was impossible and it was important to limit the damage to the economy. Unlike the compulsory lockdowns in Europe and most U.S. states, Japan’s social distancing is voluntary, even in a metropolitan city like Tokyo with a population density just as high as New York City. The number of infected and dead has been substantially lower. So far, Japan has had 15,000 cases with 500 deaths.
Several states in the U.S. have not had any form of lockdown. Media reporting has demonized the governors of these states. Clickbait headlines scare readers about the outbreaks of these states. If you dive into the numbers, though, you will see that these places are doing much better in fatality per million than New York, which has imposed a partial lockdown. South Dakota has never imposed a lockdown and, as of May 6, the state only had 2,800 positive cases with 29 fatalities.
The Unintended Consequences of Current Policies
Non-COVID-19 Patients are Suffering
The news media coverage of the COVID-19 virus and subsequent public hysteria has created precipitous drug use and halted patient visits to primary care docs and specialists for fear of being infected by COVID-19. As panic spreads, people are cancelling appointments—even critical doctor appointments and screenings. Primary care practices are seeing their patients dwindle as fear stops people from even going to the doctor. When people ignore their health, it can lead to bad outcomes and even death.
As Dr. Birx has mentioned, the death totals of patients dying from COVID-19 might be overinflated. She was referring to the concept of dying WITH COVID-19 versus dying FROM COVID-19. For example, the media has reported several incidents of children dying from COVID-19. However, these tragic deaths were results of them succumbing to other medical conditions, such as bacterial meningitis, bacterial sepsis, and Sudden Infant Death Syndrome in children who were COVID-19 positive but did not display any characteristics of COVID-19 disease.
Those who die from other causes that are COVID-19 positive are deemed to have died from COVID-19. New York City recently added several thousand to their total COVID-19 deaths even though they were not tested for COVID-19. Misinformation like this creates a sense of overblown fear and anxiety in individuals.
There has been a decrease in patient visits to hospitals and doctors’ offices. This is not just limited to elective cases or cancer screenings. With the exception of COVID-19 hotspots, data has also shown a decrease in number of ER visits by as much as 50-60%. Even the Mayo Clinic, one of the world’s leading academic medical centers, has been forced to make dramatic payroll cuts because it’s sitting with 70-80% of its beds empty.
In our nation’s push to save people from COVID-19, many patients are being neglected. Heart attacks and appendicitis aren’t magically disappearing. People still need medical care but are now too afraid to come to the hospital for fear of contracting COVID-19.
Elective Surgery is Necessary Surgery
Hospitals are denying patients elective and “non-essential” procedures because they’re waiting for COVID-19 patients who may never come. But neglecting other chronic diseases may lead to a much higher death rate than COVID-19 itself. Over 600,000 people die annually in the U.S. from heart disease and nearly that many also die from cancer. About 160,000 people die each year from Chronic Lower Respiratory Disease in the U.S. In 2017, 55,000 people died from Influenza and Pneumonia alone. If we continue to turn away people with serious illnesses, more people will die from lack of treatment than will die from COVID-19.
In addition, as patients dwindle, private practices are forced to cut costs in order to stay afloat, which frequently means laying off employees. We as a nation are creating the one thing that we tried to avoid—a shortage of people taking care of the sick. We’ve worked so hard to prevent a hospital shortage that we’ve actually created a shortage in hospital workers. As hospitals lay off physicians and nurses, this will decrease the capacity of these hospitals to take care of COVID-19 and non-COVID-19 patients. Some rural hospitals will never be able to recover from this, will go bankrupt, and will decrease access to medical care to millions of Americans. The patients are consequently suffering since they can’t get the medical help they need. In some cases, waiting to see if someone is COVID-19 positive will take too long to give them life-saving help. Just because some doctors aren’t on the front lines fighting COVID-19 doesn’t mean that they aren’t working behind the scenes to save people from other illnesses.
Our Hospitals are Hurting
It’s been estimated that at least 40,000 US healthcare workers lost their jobs in March 2020. This number will almost certainly be much larger in April 2020. When people lose their jobs and health insurance, there’s a lack of access to care. Cancer screenings will be pushed back and so will chronic illness treatments. Cancer deaths are expected to increase due to a disruption of cancer-treating services. It was recently published in the Journal of Hematology and Oncology that at least 80,000 cancers will so far have gone undiagnosed as results of our policies. These numbers will only go higher and higher the longer the lockdown continues. Once the restrictions are lifted, the backlog of screenings is going to be so immense that it will put an unprecedented strain on the already-strained healthcare system.
This will have both short and long-term impacts. With no end in sight, private practice physicians are closing their practices, and some will ultimately go bankrupt. Fewer private practice physicians and postponed elective screenings will create a bottleneck and backlog in preventative patient care. This will further delay screening procedures and increase the mortality rate even more. Ultimately, neglect of non-COVID-19 patients may kill more people than it will save.
The Economic Downturn Will Hit Small Businesses and the Poor the Hardest
As a result of these policies, we have entered a time of economic uncertainty that has not been seen since the Great Depression. Reopening the United States’ economy does not mean that all of the ultra-rich businessmen get to make millions more dollars. Large corporations like Wal-Mart, Target, Lowes, and grocery stores were deemed “essential” and never closed. While these stores do provide some “essential” services, they are drawing hordes of “non-essential” shoppers who are bored at home. Meanwhile, smaller, local grocery stores that sell the same items as these big corporations are being forced to shutter their doors. The CEO of Wal-Mart won’t suffer if some Wal-Mart’s stores close, but the owner of the corner grocery store isn’t going to be able to pay his rent or insurance now that his store has been closed. Thousands of small business owners across the U.S. are being forcibly closed, and many of them will never reopen.
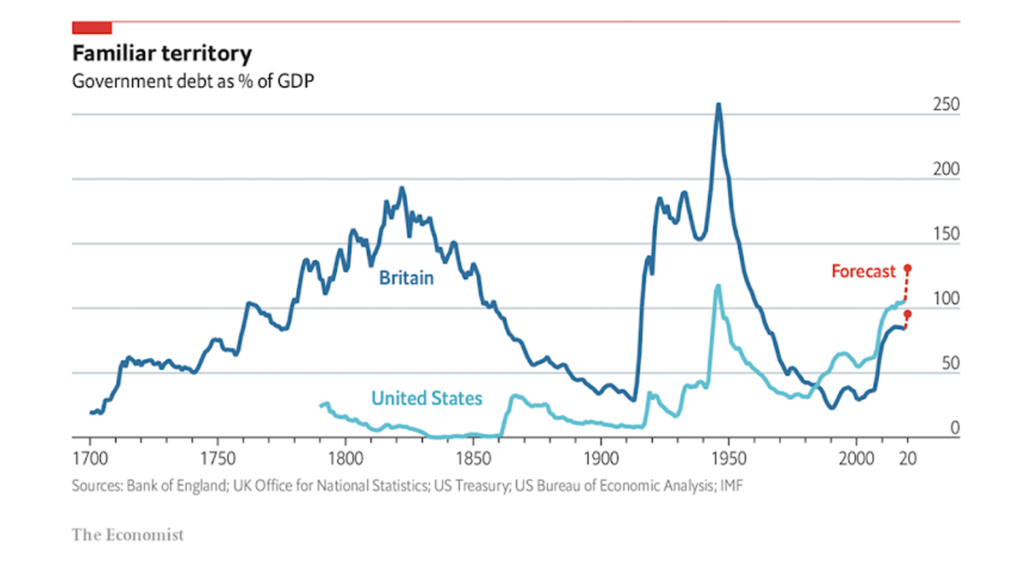
The people who are hurt the most in the economic downturn are the ones we want to protect—the poor and middle class. So far, Americans have lost 30 million jobs since shelter-in-place began. It is a fact that most of those jobs were providing health insurance for workers and their family members. Unfortunately, by losing their jobs and health insurance, these individuals will have less access to healthcare. Just one person losing her job has a ripple effect on the whole community. When 30 million jobs having been lost, it’s like dropping a boulder into a puddle.
A bad economy extends deep into our food system. Lack of jobs consequently means lack of food on the table. Reuters has estimated that over one million additional children will die this year from hunger due to COVID-19 economic woes. This shutdown affects children, especially poor children whose outlook on the future is already bleak. These kids have already missed months of school, and many of them will never get back on track. Food banks that distribute free food to those in need are already beginning to dry up. Farmers are forced to let food rot in the fields because there is no one available to pick it and distribute it. The shutdown of the economy is creating such a snowball effect that we have no idea how disastrous it will be.
Protests Have Erupted by People Seeing Empty Hospitals and Long Unemployment Lines.
Protests are building all across the nation and across the world as those who have lost their jobs and livelihoods are angry, scared, and frustrated. Many people in medicine, academia, and media chastise these protestors and call them ignorant and dangerous. Those of us in medicine and media who have a job, who are collecting a paycheck, and who don’t fear losing our family’s health insurance should not be the ones pointing fingers at individuals who are pleading for help.
Economic Suicide is a Real and Horrible Phenomenon
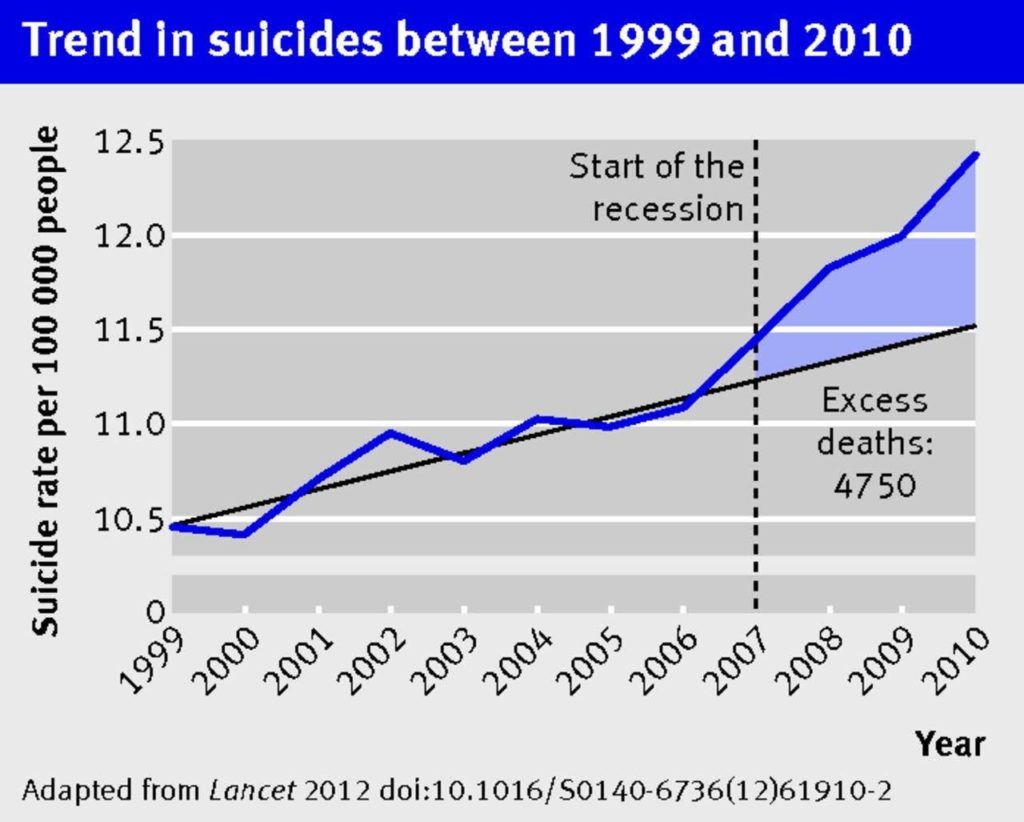
Suicides are likely going to increase as the U.S. and the world plummets toward a depression. Many factors play into a person’s decision to commit suicide, but the current state of affairs in the world will be a factor in some of them. During the Great Recession that began in 2007, suicide rates in North America and Europe rose significantly during the following years.
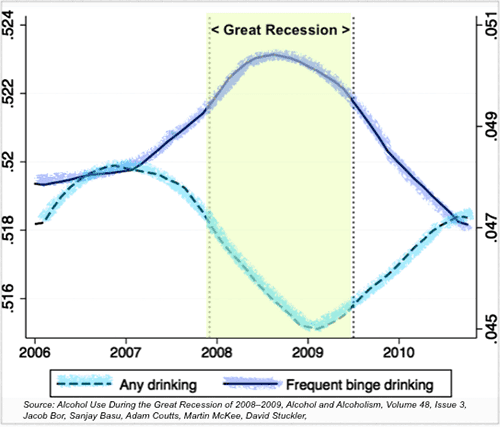
According to a study by the British Journal of Psychiatry, the two continents experienced 10,000 more suicides than in previous years. Southern California has seen an increase in calls to suicide hotlines since the stay-at-home orders began; domestic violence calls are increasing, too. Alcoholism among people stuck in lockdown is also likely to increase. The lives being lost to the COVID-19 pandemic are tragedies. But COVID-19 isn’t the only thing killing people in the United States, and some of our nation’s policies are doing more harm than good.
Steps to Take
We must acknowledge that fear and apprehension is real. There is fear of mortality and comorbidity of being affected by this virus. There is fear of getting infected and exposing those who we care most about to the virus and putting them in danger. However, just as real as those fears is the fear of economic hardship, fear of losing jobs, fear of losing one’s livelihood, fear of not being able to provide for your family fear of not being able to get the medical care that you need because of health insurance, or no access to medical care. There is fear of starvation, famine, and war as a result of economic downturn in some third-world countries. There are those of us who also fear that the policies enacted to slow down the progression of this disease may lead to far more death and devastation than the virus itself. The health of a nation and the economic health of a nation are two sides of the same coin.
In conclusion, we recommend a thorough look at the data presented here and ask those in power to examine their original biases and enact a plan to safely reopen the economy. Although thousands of lives have been tragically lost during the course of this virus, very few of them have been lost due to a lack of hospital beds, the entire premise behind the lockdown. It will take unity on the local, state, and federal government levels to place politics aside during an election year and do what is best for Americans. A better approach would be to allow schools to open and those under the age of 65 (most of the working class) to enter the workforce. They will get exposed to the disease and create herd immunity in order to protect the elderly and those with significant medical conditions who are predisposed to a higher mortality by this virus. This should coincide with informing elderly and those at high-risk to shelter in place until herd immunity is reached. State and federal governments need to supply PPEs, medicines, resources, and funding to hospitals, with close monitoring at the local level of hospital bed availability and shortages. If, at any point, data suggests that the hospital system may be overwhelmed, then talk of mitigation policies will be required. The economy needs to be reopened to get the healthcare workers the resources they need to fight COVID-19. This is the stimulus the economy needs.
As President Franklin Delano Roosevelt said, “The only thing to fear is fear itself.” Right now is when every American needs to tap into American exceptionalism. We can overcome this and we will help people in need. Meanwhile, we need to make sure that the economic engine of the U.S. can continue to run to avoid future losses. The economic health of a nation is tied to the health of a nation.
As global citizens and as doctors, our goal should always be to save as many lives as possible. The further we prolong this shutdown, the more harm it will do to our communities, our country, and our world. America needs to get back to living before we lose our way of living.
This commentary was written with Ankur J. Patel, M.D. Johnathan Geach, M.D., Jason Friday, M.D., Marisa Martin J.D. ‘21.
ANKUR J. PATEL, M.D. is a non-practicing physician based in Austin, Tex. His work in the medical device industry involves development of clinical evaluation reports for submission to notified bodies throughout the European Union.
JASON FRIDAY, M.D. is a board-certified ABPN psychiatrist and CEO of Redemption Psychiatry in Ariz. He is a graduate of the University of Arizona College of Medicine.